The first time I toured a senior living community, I walked in with a notebook full of questions and a chest full of guilt. My mom had recently been diagnosed with a mild cognitive impairment. They still made scones on Sundays and still remembered my kids' birthdays, yet she seemed confused on her daily walks and would assisted living sometimes leave the kettle running. I wished she could stay at home forever. I also wanted her safe. This afternoon has changed how I see the spectrum of senior care. What looked like a single decision at first glance turned out to be a series of flexible options that can evolve as needs change.
This is the moment many families face: the shift from doing everything yourself to building a plan. A well-planned plan is rarely created and ends in the same spot. It usually moves slowly between short-term stays, greater support and occasionally to specialized memory care. Understanding those steps, and the trade-offs at each stage, helps you protect your parent's independence while giving them the structure they need.
What families really mean when they say "We're not ready"
"I'm not ready" usually translates to three concerns: cost, loss of autonomy, and fear of a permanent move. The cost question is real and varies widely by geography and level of quality of. The loss of autonomy usually stems due to a lack of awareness about the freedom of choice is still available within senior living. Permanence is where respite care can help. A short stay gives everyone a trial period without the weight of a forever decision.
I've seen families run into trouble by waiting for a crisis. An accident, medical error or frightening wandering incident can force a rushed move, which usually costs more money and is less secure emotionally. Starting with a lighter touch, such as in-home assistance or a planned respite stay, gives you space to evaluate and adjust.
Respite care as the low-commitment bridge
Respite care is a short-term stay in an assisted living or memory care community, typically ranging from a few days to a few weeks. It could be used when your primary caregiver travels recovering from surgery or just needs a break. This isn't just for the breaks. The respite program lets your parent experience the routines of their community, meet staff, and sample activities. It also gives the care team a clearer picture of your parent's needs.
In a typical respite stay, your parent receives help with personal care, meals, medication reminders, and access to activities. Apartments with furnished rooms make life easier. There are some communities that offer respite at a daily rate, others at a weekly package. It is likely that daily rates will be over long-term month rates like the way hotels that are short-term cost less per night than a lease, but the prices will vary based on area and the level of care. If cost is tight, ask whether the community offers promotional weeks at a reduced rate during slower seasons.
Common worries surface during the first 48 hours. The mom may ask when she is "going home." Dad might miss dinner due to being uncertain of where he should place his seat. This is where staff experience plays a role. Find communities with one source of contact who checks for updates every few hours on the first day and again each morning and night over the next several days. Simple introductions and routines will help. After a week, most residents have a small circle. After two weeks, families often notice small improvements: steadier gait from regular exercise classes, higher appetite with structured meals, better sleep due to daytime engagement.
Respite is also a quiet assessment. If staff notice that your child needs a cue when bathing or is unable to stand in the shower, you learn that the bathroom setup in your home requires grab bars or a bench. If memory issues surface it is possible to prepare. A daughter I spoke to said that her dad "just needed companionship." While in respite the staff noticed that insulin doses were not being administered. That data changed the entire care plan and prevented a hospitalization.
Assisted living when life's small tasks become heavy
Assisted living sits between fully independent living and nursing-level medical care. Residents are provided with their own apartment or suite, and are assisted with daily tasks including washing, dressing, bathing, and medication management. Meals are prepared, cleaning is taken care of, and transport is provided. The emphasis is on maintaining independence without risking safety.
The best assisted living communities feel like a college campus for older adults, only slower and calmer. You can find a schedule of outings and events. There is always a card game. It is typically a group walk, chair yoga, art classes, and performances by local musicians. The most important thing is that residents can choose the amount they participate in. If your parent wants quiet mornings and a single afternoon activity, that is a perfectly valid rhythm.
Families often ask how to know it is time. I look for patterns that show missed medication frequently or more often than twice a month, weight loss because of a lack of eating, unpaid bills piling up and falls that are repeated or a caretaker who's exhausted. Another indicator of the feeling of being isolated from others. If friends do not visit and daily conversation shrinks to only a few minutes for the mail carrier Depression and cognitive decline could increase. Assisted living structures the day just enough to restart social contact.
Costs in assisted living usually combine a base rent with a tiered care fee. The basic fee covers the apartments food, the housekeeping and other activities. The cost for care increases according to the degree of support required. The community I was in utilized five levels that included level one, which was for simple medication assistance and reminders, level two for minimal support while level five provides intensive assistance throughout the day. The differences between the levels could be several hundred to over 1,000 dollars per month. A detailed assessment up front avoids surprises.
The best way to judge quality is to visit at awkward times. Visit in the middle of the morning when staffing may be less. Eat a meal. Watch how staff address residents with their names and whether they sit at eye level when speaking or addressing the agitation. Ask three residents separately what they dislike the least. If all of them mention the same thing, then it's clear what you're against. If they offer different minor complaints, that suggests overall balance.
When memory care becomes the safer lane
Memory care is designed for people with Alzheimer's disease or other dementias who need more structure and safety than assisted living can provide. It is important to consider the environment. Good memory care units have clear sight lines, secure outdoor courtyards, and cues that reduce confusion: contrasting colors on bathroom fixtures, shadow boxes outside rooms with personal photos, and simple daily schedules posted at eye level.
The goal is not to restrict, it is to scaffold. Residents still socialize, participate in arts, music and exercise, as well as go on supervised outings when appropriate. It's all in the how staff members are matched, their hands-on instruction as well as the level of training that employees get. When verbal instruction fails staff may use hands-on guidance to groom. If someone refuses to shower, a staff member could change to washcloths with warm water and then return, instead of threatening to force the matter. Small practices like offering choices ("Would you like the blue sweater or the green one?") protect dignity while moving the day along.
Families sometimes delay memory care because the word itself feels heavy. They worry their loved one will decline faster. In practice, I've often observed the reverse. People with dementia handle less choices more easily. The ability to predict reduces anxiety. This reduces behaviors like pacing, leaving, or sundowning. As anxiety decreases the appetite increases and sleep is stabilized. Those basics, multiplied day after day, can extend quality of life.
There are edge cases. A person in very early-stage dementia could benefit from assisted living with added supports. However, those with Parkinson's and mild dementia might be in need of memory care not for memory alone but for the complex medications and risk of falling. The best communities will tell you honestly which unit fits your parent's pattern of demands. If every community you tour insists they can handle anything, keep looking.
The emotional work of switching lanes
Moving a parent is not just logistics, it is loss, even when the benefits are obvious. An old-fashioned mother who led the PTA requires help showering. A father who built a business from nothing cannot recall if he had breakfast or not. The pain is. Naming that loss helps. So does involving your parent in the pieces they can choose: which photos go up, which chair to take, and which quilts to fold up towards the end to the beds. The act of packing becomes a conversation about history rather than a quiet removal of belongings.
Siblings can complicate the picture. A person may demand immediate modification, while a different one may be resistant, while a third might stay quiet. When possible, assign different roles. One handles the financial papers, another handles medical communications, and the third one oversees visits and outings. This will reduce friction and give everyone a clear contribution. If you hit gridlock, a geriatric care manager or a social worker can moderate a single family meeting to set ground rules and timelines.
Guilt rarely disappears completely. But it is possible for it to be tempered by data. Following the move, keep track of concrete indicators: weight or falls UTIs, ER visits, the amount of time you spend with other people. If these numbers rise you can use that information to inform your feelings. Parents may still be complaining about soup, or the late dinner time, and yet sleep better and get their medication in occasion. Small gripes can coexist with big gains.
Safety, independence, and the middle path
People often frame senior living as a binary: independence at home or safety in a community. However, the majority of us want both. The right setup provides safety with as much independence as is possible. That might be a studio in assisted living right next to the recreation room, so that dad is able to participate in morning games without having to take a lengthy hike. Perhaps it's the memory care apartment that opens to a safe garden, to allow your mother to manage her garden. It might be a respite stay every quarter to reset routines while staying home the rest of the year.
Autonomy shows up in choices, not in the absence of support. The choice of having breakfast later is autonomy. The decision to not take the bath, but instead opt for the warm washcloth as an act of autonomy. When capabilities change, decisions change but not the goal. I often tell families, seek out the least restrictive setting that will keep your parents safe. Revisit that aim every few months.
Medical realities that often drive transitions
Some conditions predict the need for more support. Heart failure that is advanced can cause unexpected fatigue and fall. Parkinson's disease introduces complex interactions between medications with food. The condition requires regular carb count and constant monitoring. Recurrent UTIs can worsen confusion dramatically in older adults Sometimes, it can happen in the night. When two or more of these conditions stack with cognitive loss, the tipping point comes faster.
Medication management alone can justify assisted living. Seniors with less than five medications that are taken every day, or at least once a day, could have a good time with a house medication organizer, and an annual check-in. 10 medications, including those with short timing window or frequent beehivehomes.com respite care dosage adjustments work better in a monitored setting. Communities track adherence with electronic records, something most families cannot replicate at home.
A note on hospice: it is compatible with assisted living and memory care. If your parent qualifies to be a hospice patient, the team can provide symptom management the nursing process, as well as equipment which is layered on the services of the community. I have seen hospice turn into a confusing night-time ER sequence into tranquil evenings. They are not abandoning. It is shifting goals toward comfort and dignity.
Costs, contracts, and how to avoid surprises
Money should not be a taboo topic. Ask direct questions before you sign. What is included in the basic rate? What are the different levels of care and the monthly costs? What is the frequency of reassessment, and can the level of care go down as well as increasing? How are incontinence supplies billed? Are there move-in fees or community costs? If your parent needs a helper for two persons, what's the surcharge? Are there additional charges for cognitive care programs in assisted living, separate from memory care?
Annual increases are typical. Most communities implement the 3 to 8 percent increase each year, sometimes more in high-inflation periods. An agreement should state the manner in which increases are communicated and the time they are effective. If you're concerned about cost, inquire if the community partners with long-term care insurance providers, whether it accepts certain veterans' benefits, or whether it has an emergency financial policy. Communities rarely publish discounts, but many will work within a modest range, especially if you can move during lower-demand months.
Business Name: BeeHive Homes Assisted LivingAddress: 16220 West Rd, Houston, TX 77095
Phone: (832) 906-6460
BeeHive Homes Assisted Living
BeeHive Homes Assisted Living of Cypress offers assisted living and memory care services in a warm, comfortable, and residential setting. Our care philosophy focuses on personalized support, safety, dignity, and building meaningful connections for each resident. Welcoming new residents from the Cypress and surround Houston TX community.
16220 West Rd, Houston, TX 77095
Business Hours
Monday thru Sunday: 7:00am - 7:00pm
Facebook: https://www.facebook.com/BeeHiveHomesCypress
Move-out clauses matter. If your parent is hospitalized before being transferred to a skilled nursing facility in rehabilitation, can the local community own the residence? How long and for what cost? If your parent passes away what happens to the last month prorated? These are difficult questions to ask in the sales office, but you will be grateful later that you did.
What good care looks like on an ordinary Tuesday
Grand openings are polished. Every Tuesday at 3 p.m. be honest. This is what I'm looking for on random trips. Wet floors around the dining room signal leak issues and slow housekeeping response. Residents waiting in the corridor for fifteen minutes before dinner suggest there are gaps in staffing. A clean activity calendar is inadequate. Check whether people actually go to the event and whether staff adjust to energy levels. If the posted event is a chair exercise group, but most residents look sleepy, a good facilitator changes to gentle stretches and music, not a rigid routine.
In memory care, watch for how staff respond to repetitive questions. When a patient asks her mother each time for five minutes, staff respond with patience and a grounding question ("Tell me more about your mother's garden") will prevent escalation. Staff who correct ("Your mother passed away years ago") are sincere, however they can cause stress. Consistency in tone matters as much as headcount.
Meals should feel unhurried. Patients with cognitive loss benefit from prompt, simple selections as well as visual prompts. I like to see the staff serve small portions in minutes rather than overwhelming with an enormous platter. Hydration is a quiet success driving factor. Look for water stations and staff circulating with flavored water. Dehydration is a hidden cause of confusion and falls.
How to pace decisions without losing momentum
The biggest mistakes I see are rushing without information and delaying without a plan. To balance both, set a three-step cadence.
- First, take stock at home. Note what's going well, what is dangerous, and what's draining caregivers. Be concrete. If bathing takes ninety minutes and ends in tears twice a week, write that down. Second, run two to three community tours, one of which should be a respite-capable assisted living and one a memory care unit. You should only visit unannounced every at least once. Take a bite of food at least every once. Take your parent for a short social visit if appropriate. Third, decide on a trial. Request a stay for a respite or pay a deposit with a set date to move and then set up the home with familiar items. Set measurable goals to review after two to four weeks, such as fewer falls, better sleep, or regular social engagement.
This cadence preserves your parent's voice while keeping the process moving. It also creates a structured way to debrief as a family.
Respecting identity through change
Care plans work best when they honor who your parent has always been. The retired engineer might respond well to routines and projects: sorting hardware, folding maps or building easy kits. A former teacher might thrive in reading to small groups of students or helping by playing words games. A gardener will settle down in a garden with seeds tray and pots of soil. Memory care groups worth their salt build these details into daily life. If the life story file is thin, fill it with specifics: favorite music from age 15 to 25, signature recipes, nicknames, pets, best friends, and that one travel story they tell every holiday.
Personal objects anchor memory. Bring things you'll not be worried over if they fall off such as a beloved blanket, a sturdy armchair, frames of photos, maybe postcards that depict their lives in different places. Put them in a place where they'll use them. Place the basket of knitting by your favorite chair and not on a shelf. Place the photo of your wedding on the wall at an eye-level near to the mattress. Function beats decoration every time.
A note on culture, language, and food
Communities vary in how they handle cultural preferences. Consider requesting access to a language in case your parent is comfortable in Spanish, Mandarin, Tagalog or another dialect. Some communities have bilingual staff on every shift. Other communities rely on only a couple of employees who may not always be on duty. Menus should offer choices outside of the typical American taste. If your mother grew up having congee breakfast every morning scrambled eggs might not be a good idea. Get specific with the culinary director, and consider a regular "from home" meal where family brings favorite dishes within the community's food safety rules.
Faith practices also matter. The weekly rosary circle and the Friday Shabbat lighting of candles, or a meditation circle will help you ground your week. These aren't extras. They're part of your an individual's identity. If your local community does not provide them, inquire whether you could help in organizing. Most will welcome volunteers.
When the plan changes again
A plan that starts with respite care may grow into assisted living, and later, memory care. There is also the possibility of moving in one way or the other. After a hospital stay, parents may opt to use memory care briefly for structure, then return for assisted living with additional supports. Flexible is the norm in the modern world, and not the only exception. What matters is not the labels, but how well your parent sleeps, eats, socializes, and stays safe.
Keep a quarterly check-in on the calendar with the community's care director. Bring your questions along, as well as the observations you have made during the visits. When a problem arises like missing showers or confusion with clothes bring it up early. The majority of issues can be resolved after being identified. If your patterns aren't changing despite repeated conversations, take this seriously. Good communities show you the data and then modify. If you hear only reassurance without specifics, press for a plan with dates and measurable steps.
The quiet metrics of a good decision
Families often look for a single sign they chose correctly. The odds are that there isn't one. Instead, look for a swath of silent metrics over a couple of months. It is possible that the weight will stabilize or increase little. The list of medications stops being updated every week. ER visits drop. The refrigerator at home has stopped being full of spoiled food because it is no longer needed. The conversation between your parents is less. You hear the names of new friends.
Equally important, you notice your own shoulders drop. You can sleep all night, not worrying about your phone. It's a visit with your mother or father, not as a frazzled case manager. You take a strawberry and you sit in the sun for a bit. You laugh. This isn't a sign of failure. That is care, delivered by a team, in a place designed for this exact season.
A practical word on starting
If you feel stuck, choose one next action. Call two communities and ask to be able to get respite within sixty days. If waitlists are too long and you are unsure of where to go, inquire about the places that frequently are canceled. Put all the important information in an organized file: ID and insurance card, medications lists, advance directive. Schedule a thirty-minute visit with your primary care physician to discuss care needs and medications simplification. Small steps build momentum. You do not have to solve the entire journey at once.
The path from respite care to assisted living and, when needed, to memory care is not a straight line. The path is determined by the parent's medical condition and their preferences. The ideal senior living plans preserve identity, add structure, and grow or shrink as your needs change. By paying attention to the smallest details and an openness to change, you can give your parents peace of mind without stripping of the little things that make a day feel as if it's theirs. That is the heart of senior living, and it is well within reach.
BeeHive Homes Assisted Living is an Assisted Living Facility
BeeHive Homes Assisted Living is an Assisted Living Home
BeeHive Homes Assisted Living is located in Cypress, Texas
BeeHive Homes Assisted Living is located Northwest Houston, Texas
BeeHive Homes Assisted Living offers Memory Care Services
BeeHive Homes Assisted Living offers Respite Care (short-term stays)
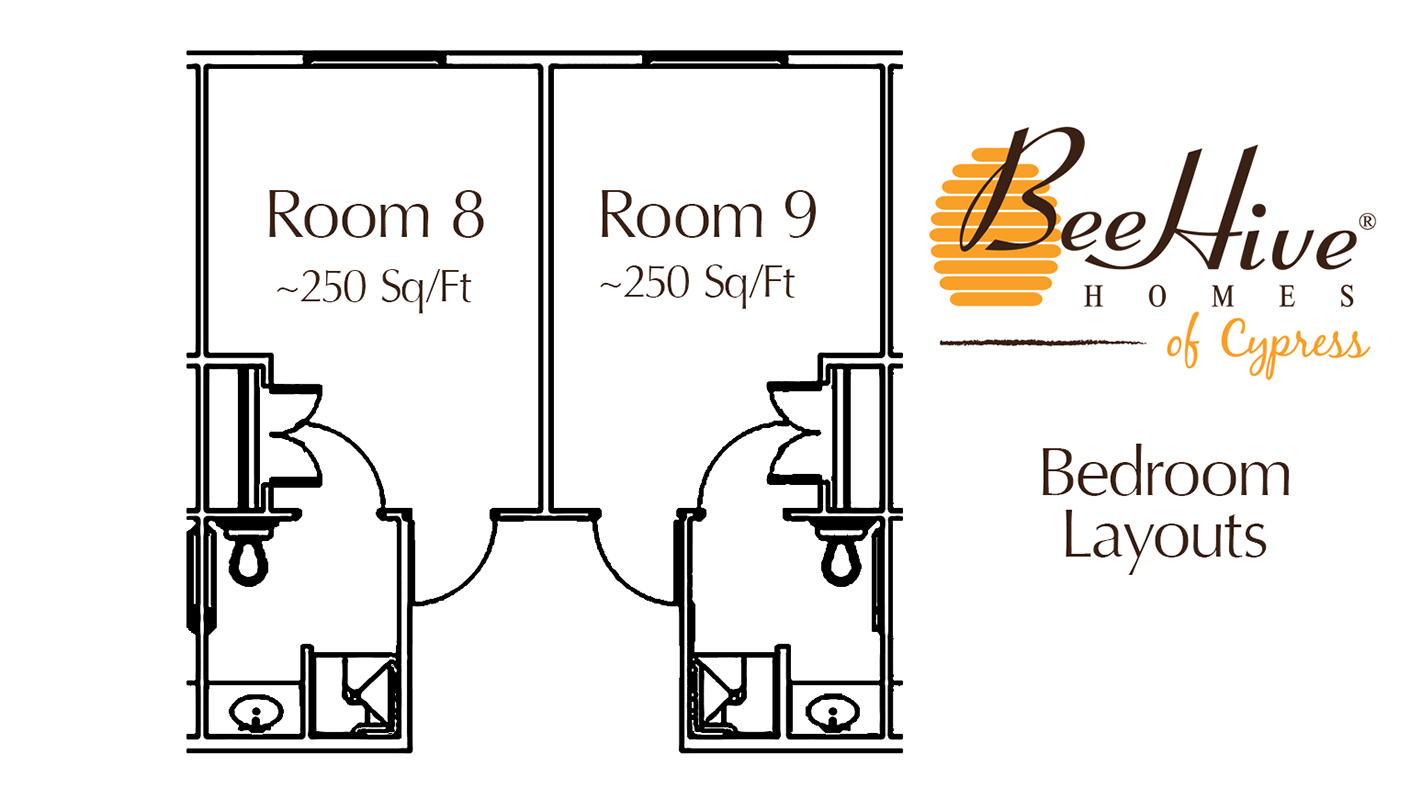
BeeHive Homes Assisted Living provides Private Bedrooms with Private Bathrooms for their senior residents
BeeHive Homes Assisted Living provides 24-Hour Staffing
BeeHive Homes Assisted Living serves Seniors needing Assistance with Activities of Daily Living
BeeHive Homes Assisted Living includes Home-Cooked Meals Dietitian-Approved
BeeHive Homes Assisted Living includes Daily Housekeeping & Laundry Services
BeeHive Homes Assisted Living features Private Garden and Green House
BeeHive Homes Assisted Living has a Hair/Nail Salon on-site
BeeHive Homes Assisted Living has a phone number of (832) 906-6460
BeeHive Homes Assisted Living has an address of 16220 West Road, Houston, TX 77095
BeeHive Homes Assisted Living has website https://beehivehomes.com/locations/cypress
BeeHive Homes Assisted Living has Google Maps listing https://maps.app.goo.gl/G6LUPpVYiH79GEtf8
BeeHive Homes Assisted Living has Facebook page https://www.facebook.com/BeeHiveHomesCypress
BeeHive Homes Assisted Living is part of the brand BeeHive Homes
BeeHive Homes Assisted Living focuses on Smaller, Home-Style Senior Residential Setting
BeeHive Homes Assisted Living has care philosophy of “The Next Best Place to Home”
BeeHive Homes Assisted Living has floorplan of 16 Private Bedrooms with ADA-Compliant Bathrooms
BeeHive Homes Assisted Living welcomes Families for Tours & Consultations
BeeHive Homes Assisted Living promotes Engaging Activities for Senior Residents
BeeHive Homes Assisted Living emphasizes Personalized Care Plans for each Resident
People Also Ask about BeeHive Homes Assisted Living
What services does BeeHive Homes of Cypress provide?
BeeHive Homes of Cypress provides a full range of assisted living and memory care services tailored to the needs of seniors. Residents receive help with daily activities such as bathing, dressing, grooming, medication management, and mobility support. The community also offers home-cooked meals, housekeeping, laundry services, and engaging daily activities designed to promote social interaction and cognitive stimulation. For individuals needing specialized support, the secure memory care environment provides additional safety and supervision.How is BeeHive Homes of Cypress different from larger assisted living facilities?
BeeHive Homes of Cypress stands out for its small-home model, offering a more intimate and personalized environment compared to larger assisted living facilities. With 16 residents, caregivers develop deeper relationships with each individual, leading to personalized attention and higher consistency of care. This residential setting feels more like a real home than a large institution, creating a warm, comfortable atmosphere that helps seniors feel safe, connected, and truly cared for.Does BeeHive Homes of Cypress offer private rooms?
Yes, BeeHive Homes of Cypress offers private bedrooms with private or ADA-accessible bathrooms for every resident. These rooms allow individuals to maintain dignity, independence, and personal comfort while still having 24-hour access to caregiver support. Private rooms help create a calmer environment, reduce stress for residents with memory challenges, and allow families to personalize the space with familiar belongings to create a “home-within-a-home” feeling.Where is BeeHive Homes Assisted Living located?
BeeHive Homes Assisted Living is conveniently located at 16220 West Road, Houston, TX 77095. You can easily find direction on Google Maps or visit their home during business hours, Monday through Sunday from 7am to 7pm.How can I contact BeeHive Assisted Living?
You can contact BeeHive Assisted Living by phone at: 832-906-6460, visit their website at https://beehivehomes.com/locations/cypress/,or connect on social media via Facebook
BeeHive Assisted Living is proud to be located in the greater Northwest Houston area, serving seniors in Cypress and all surrounding communities, including those living in Aberdeen Green, Copperfield Place, Copper Village, Copper Grove, Northglen, Satsuma, Mill Ridge North and other communities of Northwest Houston.